This document was passed out at the Preparation meeting last week, the panel went over it page by page. I am going to comment page by page.
The Work group pointed out that while these "answers" were given to CMS from HSD the workgroup members don't think that Leadership should be satisfied with the answers given. A Tribal Leader needs to ask CMS in front of HSD if CMS is satisfied with the answers in this Response.
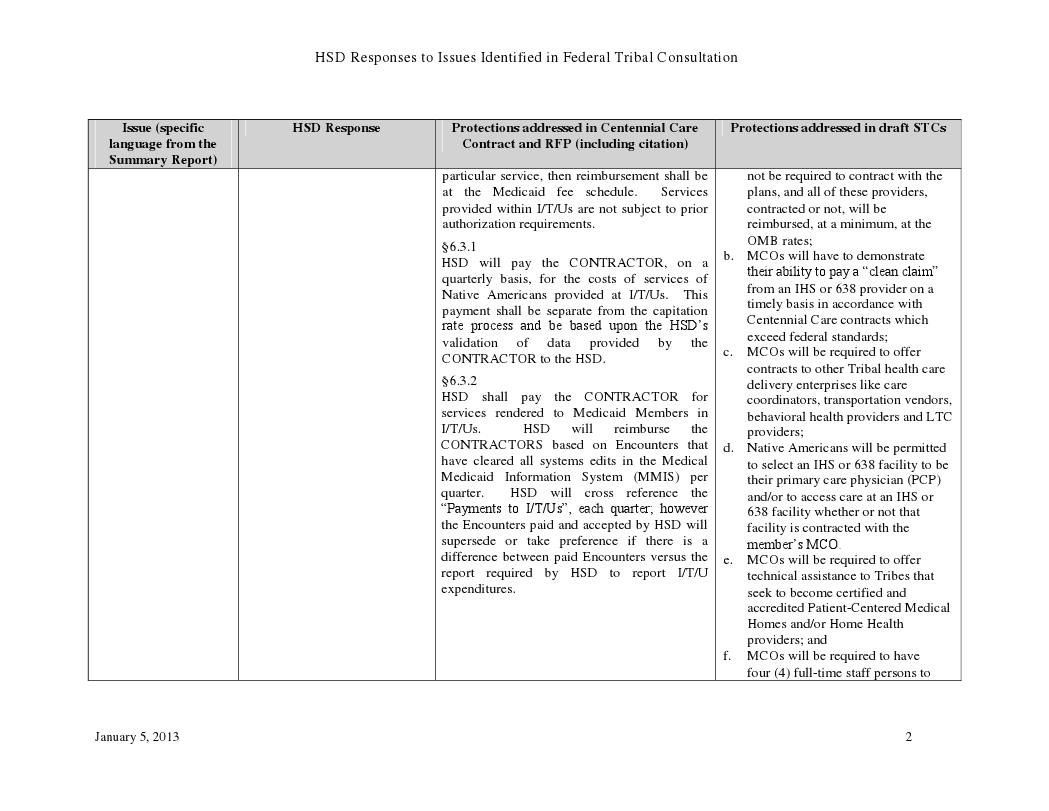
"HSD Responses to Issues Identified in Federal Tribal Consultation"
Page 1: In the Last Column regarding the Native American Advisory Board and the Native American Technical Advisory Board, a subcommittee of the NM MAC, Tribes should appointment their own representatives to these two boards not HSD, MAD,IAD or the Governors Office.
The NATAB has already been formed and has been meeting, the board was appointed by Julie Weinberg of NMMAD and does not have direct representation by Tribe.
Third column: 6.3.1 Many of the Workgroup members feel that Tribal Leadership needs to ask for Clarification on this statement, it sounds like the CONTRACTOR (MCO) is being paid twice for the NA population.
Last column section c. Other Tribal Health care Delivery Enterprises should be allowed the same access to the 100% FMAP funding mechanism that IHS and 638 Facilities have.
Second Column: Centennial Care will create five new separate Systems that Tribes will have to interface with and be able to navigate each plans approved provider network, for entire Medicaid population, creating a huge Administrative Burden. Comprehensive care coordination and oversight measures are already in place through the IHS and 638 Clinics.
Third Column: How will HSD/MCOs Identify these populations?
Third Column: under Issue #4 Needs clarification on Reimbursements in I/T/Us, why are there exclusions to services that are reimbursable, and is the OMB fee rate different than the Medicaid fee rate?
First Column: second paragraph, this is a false statement many rural communities in NM lack the available provider network and MCO presence, making access difficult.
Third Column: 4.412.2, Reimbursement needs to go to the I/T/Us for care coordination functions, I/T/Us do the work they should get paid for it.
Second Column: Needs clarification of statement " improve access issues by fostering and providing incentives for innovative approached to service delivery such as the use of mobile unit" what do they mean by "incentives"
Third column: 4.4.2.7 this statement needs to addressed basically it says that an MCO only needs to make three attempt to reach a member twice by phone, once by letter, and that will constitute "sufficient effort" to reach a member, capitated PMPM payment will still be automatically made to MCO on behalf of that unreachable member.
Second Column: issue #1 (page8) still need clarification on how a NA will identify themselves as a Tribal member.
Second Column: issue #1 (page9) this is a non-answer this is the way that the system is currently set up and there are rampant payment/reimbursement issues from the MCOs
Second column: started on previous page, another non-answer from HSD tribes have shown and proven that the elimination of retroactive payment will have a huge effect tribal CHS budget, the assumption by HSD is that mandatory enrollment into Centennial Care or HIX or private insurance would negate the need for retroactive payment, the protections afforded to NA by the PPACA and IHCIA and ARRA show that NA are excluded from mandatory inclusion.
second column Issue #1 (page9) this is a non-answer also, putting the burden of responsibility on the MCO to adhere to the contract requirements does not answer the question.













No comments:
Post a Comment