From the Center on Law and Poverty:
Dear Tribal Leaders:
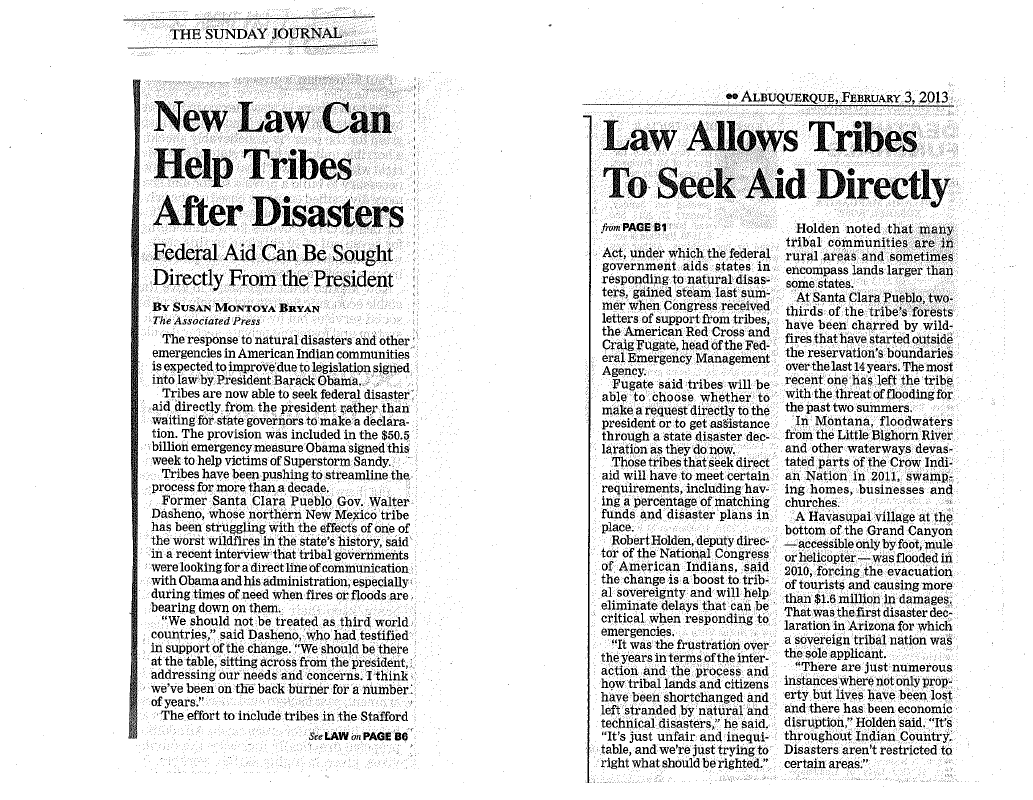
On Friday, February 1 following Indian Day ceremonies, a number of leaders and tribal workers met to discuss strategy related to the state’s pending request of the Centers for Medicare and Medicaid Services (CMS) for an 1115 Waiver which would allow the state to implement Centennial Care. It was acknowledged that pressure needs to be applied to CMS to convince Director Cindy Mann (410-786-3871) to disallow the requirement that Native people be automatically enrolled in managed care organizations and that the fee-for-service reimbursement arrangement that Native health care facilities have used successfully for many years remain in place. Santa Clara Governor Tafoya proposed that calls be placed to President Obama at the White House (202-456-1111) to inform him of the tribes’ positions regarding the MCO enrollment requirement and the need for the fee-for-service arrangement. He cited the President’s recent response to natural disasters and other emergencies on tribal lands whereby tribes can now “seek federal disaster aid directly from the president rather than waiting for state governors to make a declaration (Albuq. Journal, Feb. 3, 2013, attached). Tafoya’s proposal echoed the position taken by Mescalero Tribal Administrator Freddie Kayadazinne who highlighted the commerce clause of the Constitution that establishes the arrangement for federal/tribal relations. In the newspaper article that reported the new provision for direct requests to the President, former Santa Clara Governor Walter Dasheno stated that “[w]e should not be treated as third world countries” but rather “[w]e should be there at the table, sitting across from the president, addressing our needs and concerns.” All those present at the meeting agreed that health care services are among the most important resources that must be safeguarded.
The second proposal involved HB 376 which was recently introduced by Representative James Roger Madalena from Jemez. The bill seeks to enact a “new section of the Public Assistance Act to remove Native Americans from mandatory enrollment in Medicaid managed care.” The group decided that the more effective route to remove the mandatory enrollment requirement is an amendment to a “section of the Public Assistance Act to ban mandatory enrollment of Native Americans in Medicaid managed care.” A substitute bill was drafted. Copies of both bills are attached. Hearings on the substitute bill will be held by the House Judiciary Committee and House Health, Government and Indian Affairs Committee. It is essential that as many people as can show up for these hearings. We need to pack the rooms with Indians. I will keep on top of this and send word out about date, time and place of these hearings. Those of you who know how to track legislation will be able to do this yourselves. Attached are lists of committee members and their phone numbers. It is difficult to organize the call-in but if each member of both committees could receive at least ten calls a day from tribal and off-rez locations that would go a long way to convince the legislators that the people are deeply serious about their objections to state-imposed managed care services. Family members and friends can join in the effort. The procedure is simple. The caller will give her/his name, the location from which the call is being made and a statement that the caller supports passage of HB 376. Calls to legislators’ offices are answered by administrative staff who keep a tally of the calls, supporting/not supporting.
The third approach concerns the introduction of a memorial that states the tribes objections to managed care that can be passed by the full legislature. A memorial will communicate to CMS that the state legislature recognizes the validity of the tribes’ objections. This document is being prepared by Ken Lucero, AIPC Health Committee Chairman. As soon as it is completed, I’ll send it out to you. A talking points document was also prepared and is attached.
At the meeting Ken pointed out the fallacy of the state’s position that managed care will save money. He cited the example of the planned five managed care contracts that will be let. If each of these managed care companies enrolls different members of the same tribe that will mean that the companies will be required to employ a total of five separate care coordinators. The care coordinator is the lynch pin of the success of the managed care arrangement. A managed care enrollee will receive a health care assessment which will give direction to the health care services package that the company will provide. The care coordinator will oversee the provision of services for each enrollee to assure that the enrollee receives the services to which he/she is entitled. These are complex responsibilities that include sophisticated comprehension of the cultural landscape of health care delivery in Indian country.
Another area of serious concern is the reimbursement problems that both the Indian Health Service and tribal/off-rez facilities confront. For example, OptumHealth was awarded the contract for behavioral health services in 2009 and began work in 2010. In just three years of operation, Indian Health Service and the tribal and urban programs have been subjected to unpaid accounts in the amount of $900,000. These are monies that the facilities need to buy pharmaceuticals, pay provider salaries, support facilities and operations, etc. These delinquencies are unacceptable and interfere with the ability of tribes and off-rez health care facilities to provide care and services for their consumers and patients.
There is much that we can do to accomplish the goals that have been set forth. Please contact me if I can be of help with the various tasks described. This is a winnable endeavor.
Best regards,
Evelyn Blanchard
Organizer



No comments:
Post a Comment